Preventing Microbial Contamination During Pharmaceutical Manufacturing
- Direct costs related to batch rejections and product recalls
- Loss or endangerment of human lives
- Damage to company's reputation
- Facility - flow of personnel, material, waste etc.
- Equipment - Assembly, cleaning, sterilization
- Processes
- Raw materials
- Personnel - shedding cells, skin, oils, hair, clothing etc.
- Environment
- Personnel
- Critical surfaces
- container/closure sterilization and transfer procedures
- Maximum product holding before filling into the final container
- Sterilizing processes
- 21CFR 211.28 - provides guidance on the use of protective apparel
- 21CFR 211.42 - provides guidance for the proper facility design and placement of equipment
- 21CFR 211.67 - equipment cleaning, sterilization, and maintenance
- 21CFR 211.100 - production and process controls
- 21CFR parts 600-610 - applicable regulations for therapeutic recombinant products and monoclonal antibodies
- Points to consider in the Manufacture and Testing of Monoclonal Antibody Products for Human Use published in February 1997,
- Guidance on Viral Safety Evaluation of Biotechnology Products Derived From Cell Lines of Human or Animal Origin (Q5A),
- Guidance on Quality of Biotechnological/Biological Products: Derivation and Characterization of Cell Substrates Used for Production of Biotechnological/Biological Products (Q5D),
- Guidance on Specifications: Test Procedures and Acceptance Criteria for Biotechnological/Biological Products (Q6B)
If you are involved in pharmaceutical product manufacturing, you have the responsibility to ensure the quality of the product being manufactured. You must closely adhere to the carefully established and validated methods of preparation and procedures.
Microbial contamination of drug products is one of the frequently cited FDA observations. Consequences of microbial contamination can include:
So, it is important to understand the causes of microbial contamination in drug product manufacturing. Acquiring this knowledge will not only help manage risk better, but also establish effective mitigation strategies.
Microbial Contamination Sources in Drug Products Include
A Reference from Actual FDA Warning Letters
1. Your firm failed to establish and follow appropriate written procedures that are designed to prevent microbiological contamination of drug products purporting to be sterile, and that include validation of all aseptic and sterilization processes (21 CFR 211.113(b)).
Poor Aseptic Behavior
On May 23, 2017, our investigator observed multiple poor aseptic practices during the set-up and filling of (b)(4) batch (b)(4).
For example, during the aseptic filling of vials, an operator used restricted access barrier system (RABS) (b)(4) to remove a jammed stopper by reaching over exposed sterile stoppers in the stopper bowl. The RABS (b)(4) disrupted the unidirectional airflow over the stopper bowl, creating a risk for microbial contamination. After the operator removed the jammed stopper, the filling line was restarted, but the affected stoppers were not cleared.
In your response, you included revised aseptic technique procedures for set-up and filling. However, your response was inadequate because you did not perform a retrospective investigation and thorough risk assessment of the effect on your product. In addition, your revised procedure FF21024 permits contamination of product-contact surfaces during set-up, followed by wiping with a disinfectant, instead of preventing sterile equipment contamination by improved design and procedures.'
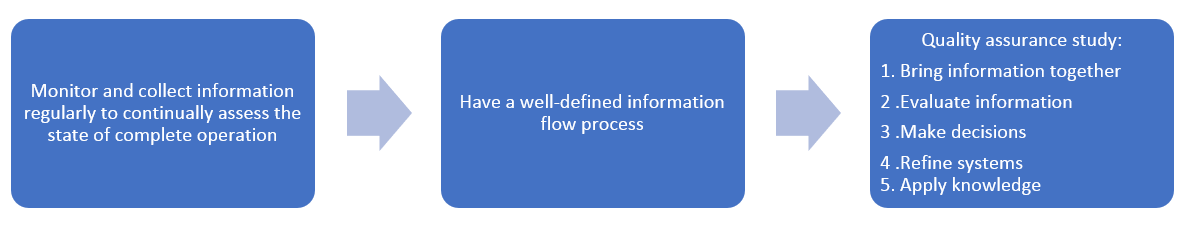
The Quality Assurance Process
You can start the quality assurance process in the early stages of drug development even when you do not have information about a lot of specific processes. As the development progresses, you can start building knowledge about the process. Both during the early development stage and at all stages, it is important that you largely have the same sterility assurance requirements.
The Scope of Quality Assurance
Rather than emphasizing quality assurance only in the end product testing, quality assurance should be built into the operations and processes. It should be included in all aspects of processing, including preparation and facilities.
A control strategy should be in place to prevent microbial contamination in all operating conditions and the treatment of materials. (Quality Assurance of Pharmaceuticals 2007). The assessment of the output of control systems should then be carried out as part of the lot disposition process.
The following factors must be included in the control strategy to preserve the sterility of the components and the product during aseptic processing:
Tools to Help You Learn How to Prevent Microbial Contamination Discrepancies
To mitigate the risk of non-compliance, manufacturers will find it useful to understand
How to create a FDA-compliant microbial contamination control program
Microbial Contamination Control in Aseptic and Non-Sterile Manufacturing
How to effectively resolve problems like recurring micro failures, investigations, and ineffective CAPAs
Testing of raw materials for microbial presence
The Microbial Factor of Non-Sterile Cleaning Validation
Signup for the relevant training programs by clicking on the links above.
Regulations and Guidance
21CFRB'211 provides the Current good manufacturing practice (CGMP) minimum requirements for preparation of finished human drug products.
The guidance on CGMP for active pharmaceutical ingredients, Q7A
Additional documents
This site provides the knowledge and teaches regulatory compliance professions the skills they need to ensure quality and compliance. This is just one of the many tools and resources you'll find here at ComplianceOnline. Subscribe to our free newsletter, or attend our webinars, seminars, or courses and really supercharge your performance.