Starting a Sustainable Healthcare Compliance Program - Information for Healthcare Providers
The healthcare compliance affects every type of provider from a solo practitioner to the largest global healthcare conglomerate. With soaring medical fraud rates, there is an increase in governmental inquiries, audits and investigations. Enforcement actions against hospitals, doctors and other provider types demonstrates financial penalties, fines, settlements and even imprisonment are on the rise. A compliance program can be to your organization's benefit if something does go wrong and you are investigated by enforcement agencies.
What is healthcare compliance program?
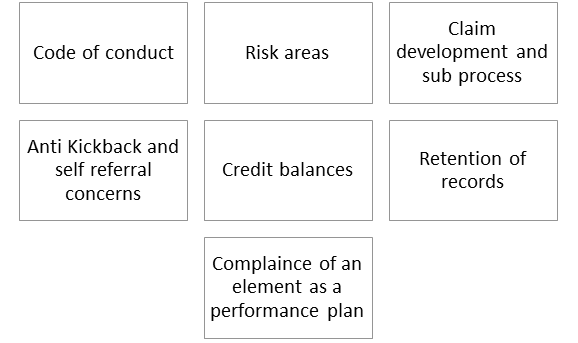
It is a program that requires healthcare organizations to develop effective processes, policies, procedures to define code of conduct in written form. The program requires the organization's staff to be trained and monitored for adherence to the defined processes, policies, and procedures.
Such a compliance program helps the organization meet or exceed the legal, ethical, and professional standards required of a healthcare organization. With the ever-evolving volume of regulations for healthcare organizations and providers, a large organization or provider requires a dedicated team to focus on healthcare compliance.
According to the OIG, an effective compliance program must at least address the following 7 elements:
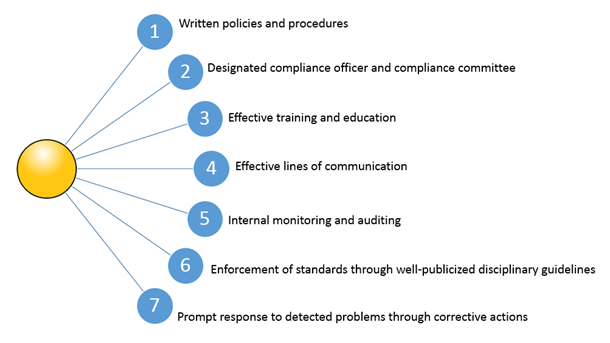
- Written policies and procedures:
- Designated Compliance officer and compliance committee
- Effective training and education
- Qualified trainers
- Training general and relevant to the staff's responsibilities
- Training appropriate and adequate to cover the range of issues confronting employees
- Adapt any changes in Federal healthcare program into training program
- Include takeaway points from results of audits and investigations; results from previous training and education programs; trends in hotline reports; and OIG, CMS, or other agency guidance or advisories
- Consider frequency, length, delivery via live instructors or via computer based
- Gather feedback after training program, steps to ensure attendees understand and retain the subject matter delivered
- Training on fraud and abuse laws
- Document who completed required training
- Whether to impose sanctions for failing to attend training or to offer appropriate incentives for attending training
- Effective lines of communication
- A culture that encourages open lines of communication, without fear of retaliation
- A hotline for staff, contractors, patients, visitors, and medical and clinical staff members to report potential compliance issues
- Good publicity of hotline, call logs and tracks to establish patterns, informing caller of hospitals action
- Investigations of fraud and abuse and sharing of the results of investigations with the governing body and other departments regularly
- Finding remedies to institutional or recurring problems with governing body's active participation
- Use of alternative communication methods such as newsletters or compliance intranet
- Internal Monitoring and Auditing
- Determine the frequency of the audits
- Address the proper areas of concern
- Assessment of billing and claims accuracy to identify root cause of billing errors
- Clear establishment of the roles of auditors
- Qualified Independent coding and audit personnel
- Availability of audit department to conduct unscheduled reviews
- A mechanism that allows compliance department to request additional audits or monitoring if needed
- Evaluation of error rates in annual audits
- Review of billing documentation including clinical documentation, in support of the claim
- Enforcement of standards through well-publicized disciplinary guidelines
- Incentives to perform in line with the compliance program
- Disciplinary measures for violation and for failing to take reasonable steps to prevent or detect criminal conduct.
- Prompt response to detected problems through corrective actions
- Take steps to correct the problem
- Also look at how your current program can be adjusted to prevent the issue from recurring.
The program should require the development and distribution of written compliance policies that identify specific areas of risk to the hospital. These policies should be developed under the direction and supervision of the chief compliance officer and compliance committee, and, at a minimum, should be provided to all individuals who are affected by the particular policy at issue, including the hospital's agents and independent contractors.
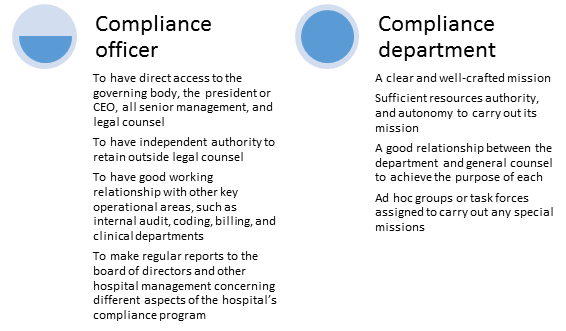
'The compliance department should be led by a well-qualified compliance officer, who is a member of senior management, and should be supported by a compliance committee. The purpose of the compliance department is to implement the hospital's compliance program and to ensure that the hospital complies with all applicable Federal health care program requirements.'
Factors to consider:
'The purpose of conducting a training and education program is to ensure that each employee, contractor, or any other individual that functions on behalf of the hospital is fully capable of executing his or her role in compliance with rules, regulations, and other standards.'
Factors to consider:
Open communication is an essential part of an effective compliance program.
Points to consider while assessing hospital's ability to communicate potential compliance issues effectively
Just like regular health checkups for humans, compliance program should be regularly audited to check upon its relevance and effectiveness
Factors to consider:
Outline a plan on how you intend to enforce the compliance program starting with how you plan to distribute and train your staff on the policies and procedures. Promote the organization's compliance program and enforce it consistently throughout the organization
The corrective action plan should clearly state how compliance violations should be identified, confirmed and handled - from who needs to be notified to what disciplinary action needs to be taken.
How the healthcare compliance program benefits your organization
- Having a compliance program significantly advances the prevention of fraud, abuse and unethical conduct. It furthers the fundamental mission of the hospital, which is to provide quality care to patients.
- It gives an opportunity to concretely demonstrate to employees and the community at large the organization's strong commitment to be an honest and responsible provider and corporate conduct.
- It provides a centralized source for distributing information on health care statutes, regulations and other program directives related to fraud and abuse and related issues. Compliance is a requirement. A compliance program demonstrates your adherence. Section 6401 of the Affordable Care Act provides that a "provider of medical or other items or services or supplier within a particular industry sector or category" shall establish a compliance program as a condition of enrollment in Medicare, Medicaid, or the Children's Health Insurance Program (CHIP).
Attend the seminar 'How to start a Healthcare Compliance Program' to take a deep-dive into the current regulatory enforcement environment in the health care industry, Review recent settlement cases due to a lack of compliance, analyze and apply the 7 elements of an effective compliance program as defined by the U.S. Sentencing Guidelines, Understand the Role of the U.S. Health and Human Services Office of Inspector General in regards to Compliance Programs, Review principles of and effective compliance program and Summarize skills and roles of a Chief Compliance Officer.
The speaker C.J. Wolf, MD, M.Ed. has been involved in healthcare for over 20 years beginning with his years in medical school. He has worked in various coding, reimbursement or Chief Compliance Officer Roles for Intermountain Healthcare, the University of Texas MD Anderson Cancer Center, the University of Texas System and Merit Medical Systems. He currently is Sr. Compliance Executive at Healthicity.






